Author Archives: Mark Ilhan

Oakwood Labs is happy to announce that we will be exhibiting at Booth #748 at the upcoming 2025 Convention on Pharmaceutical Ingredients (CPHI) on May 20-22 in Philadelphia, Pennsylvania. If you would like to learn more about the event and register to attend, please visit the following link: https://www.cphi.com/americas/en/home.html
Company Overview
Oakwood Labs is a global leader in sustained release drug delivery. We support all phases of long acting injectable development from initial feasibility studies through FDA-approved clinical and commercial supply. Oakwood has 28 years of drug encapsulation experience using Chroniject™, our patented microsphere-based technology. Chroniject™ provides the ability to control particle size, customize release durations from weeks to years, and minimize residual solvents to achieve critical quality attributes.
Stop by Oakwood Lab’s Booth #748 to meet our team and learn more about how we can assist in the following areas:
- Long Acting Injectable Technology (CDMO)
- Feasibility studies
- Scale-up and optimization of formulation
- Manufacturing GLP toxicology batches
- Clinical trial manufacturing (Phase I, II, III)
- Contract Manufacturing (CMO)
- Technology Transfer
- GMP Registration and Validation batches
- Aseptic GMP commercial batch manufacturing
- ICH compliant stability testing
Contact Us for More Information
The CPHI Americas 2025 conference covers a wide range of topics, and we are happy to contribute to the event! If you aren’t able to attend, but still want to learn more about Oakwood Labs or what you missed at the conference, contact us today!
We look forward to discussing our technology and more.
Oakwood Labs is happy to announce that we will be exhibiting at Booth #2030 at the upcoming 2025 Association for Research in Vision and Ophthalmology (ARVO) on May 4-7 in Salt Lake City, Utah. If you would like to learn more about the event and register to attend, please visit the following link: https://www.arvo.org/annual-meeting/
Company Overview
Oakwood Labs is a global leader in sustained release drug delivery. We support all phases of long acting injectable development from initial feasibility studies through FDA-approved clinical and commercial supply. Oakwood has 27 years of drug encapsulation experience using Chroniject™, our patented microsphere-based technology. Chroniject™ provides the ability to control particle size, customize release durations from weeks to years, and minimize residual solvents to achieve critical quality attributes.
Stop by Oakwood Lab’s Booth #2030 to meet our team and learn more about how we can assist in the following areas:
- Long Acting Injectable Technology (CDMO)
- Feasibility studies
- Scale-up of formulation
- Manufacturing toxicology batches
- Clinical trial manufacturing (Phase I, II, III)
- Contract Manufacturing (CMO)
- Technology Transfer
- GMP Registration and Validation batches
- Aseptic GMP commercial batch manufacturing
- ICH compliant stability testing
Contact Us for More Information
The ARVO 2025 conference covers a wide range of topics, and we are happy to contribute to the event! If you aren’t able to attend, but still want to learn more about Oakwood Labs or what you missed at the conference, contact us today!
We look forward to discussing our technology and more.
The pharmaceutical industry harbors a vast range of key facts and significant data that can be beneficial to individuals and companies in the field. With the pharmaceutical market on a continuous rise in terms of revenue, innovation, and research, it’s important to stay up to date on current trends.
That’s why our team has compiled a list of 40+ statistics for your review, so you can learn more about the thriving pharmaceutical sector.
General Pharmaceutical Industry Trends
- New modalities, like cell and gene therapy, have increased from 11% to 21% of the drug development pipeline (McKinsey & Company)
- Based on pharmaceutical sales, the top therapeutic areas in the pharma industry are antidiabetics, immunology, oncologics, HIV antivirals, and respiratory (Statista)
- Research and development spending reached more than 300 billion dollars in the United States in 2023 (Statista)
- In 2023, biotechnology contributed to 40% of global pharmaceutical sales (Statista)
- The process of developing a new drug costs around 2.6 billion dollars in the USA, with the drug taking an average of 15 years to develop (Statista)
- The Pharmaceutical Research and Manufacturers of America trade group spends 21% of their revenue on research and development (Statista)
- PhRMA member companies spent 96 billion dollars in the USA on research and development in 2023 (Statista)
- In 2023, more than 5,500 pharmaceutical companies were conducting active research and development (Statista)
- More than 21,000 drugs were in the research and development phases in 2023 due to COVID-19 responses (Statista)
- Pfizer was the top U.S. company to develop new drugs in 2024 (Statista)
Statistics About the Pharmaceutical Market
- The total global pharmaceutical market in 2023 was estimated at around $1.6 trillion (Statistica)
- Compared to 2022, the total global pharmaceutical market increased by over 100 billion dollars in 2023 (Statistica)
- The United States accounts for nearly 40% of the world’s pharmaceutical market (National Library of Medicine)
- As of 2023, the top 5 largest pharmaceutical companies were Eli Lilly ($578.3B), Novo Nordisk ($452.8B), Johnson & Johnson ($377.7B), Merck ($263.9B), and AbbVie ($261.2B) (Visual Capitalist)
- Approximately $60 billion is spent collectively by the top 20 pharmaceutical companies each year for drug development (McKinsey & Company)
- The United States accounts for roughly 50% of global pharmaceutical sales revenue (PharmaNewsIntelligence)
- The pharmaceutical market in the United States is expected to surpass $1 trillion by the year 2030 (American Pharmaceutical Review)
- The biopharmaceutical market is expected to reach nearly $517 billion in 2024, and reach up to almost $762 billion by 2029 (Modor Intelligence)
- From 2024 to 2028, the pharmaceutical market is projected to experience an increased annual growth rate of 5.96% (Statistica)
- By 2027, the total global spending on medicine is projected to reach $1.92 trillion (Statistica)
- Currently, the United States is looking for an increased demand for personalized medicine and more targeted therapies (Statistica)
- In 2024, the United States gained more than 760 billion dollars in revenue from the pharmaceutical market (Statista)
- The United States accounted for 52% of global sales in the global pharmaceutical sector in 2024 (Statista)
A Career in the Pharmaceutical Industry: Noteworthy Statistics
- 56.8% of pharmacists in the United States are women and 43.2% of pharmacists are men (Zippia)
- Approximately 1.3 million people are employed in the pharmaceutical industry in the United States (U.S. Bureau of Labor Statistics)
- The average age of a pharmacist is 41 years old (Zippia)
- 91% of graduated pharmacists are known to work in the private sector (NIH)
- The average salary of a pharmacist is $118,968 as of 2024 (Zippia)
- The highest paying state for pharmacists is California, where the average yearly salary is $161,597 (Zippia)
- For every dollar that a man makes as a pharmacist, a woman makes approximately 98¢ (Zippia)
- The employment for pharmacists is expected to grow by 3% from 2022 to 2032 (U.S. Bureau of Labor Statistics)
- Over the decade, there is said to be 13,400 openings for pharmacists projected each year (U.S. Bureau of Labor Statistics)
- There has been a 20% increase in the demand for STEM-related jobs, making it difficult for the pharma industry to recruit technical talent (McKinsey & Company)
Statistics on Popular Prescription Drugs
- According to the Centers for Medicare & Medicaid Services (CMS), out-of-pocket drug spending is projected to peak in 2023 at $52.5 billion (Peterson-KFF)
- As of July of 2023, 25% of adults who take prescription drugs report difficulty in affording their medication (Peterson-KFF)
- There are more than 32,000 generic drugs that are approved by the FDA as of 2022 (FDA)
- In the United States, 91% of prescriptions are filled as generic drugs (FDA)
- Nationwide, the total spending on prescription drugs increased from $30 billion in 1980 to $335 billion in 2018 (Congressional Budget Office)
- Though the top 10% of drugs by price account for less than 1% of all prescriptions, they make up 15% of the retail spending and anywhere from 20% to 25% of the nonretail spending (ASPE)
- In 2020, around 6.3 billion prescriptions were dispensed in the United States (Statistica)
Oakwood Labs: Innovator of Sustained Release Drugs for the Pharmaceutical Sector
As seen in these compelling pharma market insights, it’s clear that the pharmaceutical industry is continuing to expand and develop, providing great value for both patients and business alike. Oakwood Labs plays an important role in this growth as a leader in the design and development of sustained-release drugs.
By using Chroniject™ technology, we developed a process where small molecules, peptides, and proteins can be injected and released over weeks, months, or years. This technology supports innovative solutions and has contributed to the success of the pharma industry.
With over 25 years of experience, we’ve helped bring drugs to the pharmaceutical market that enhance patient care and greatly benefit organizations. We also work with a wide range of clients, supplying services such as:
- Analytical and stability testing
- GMP aseptic manufacturing
- Feasibility program
- Formulation optimization and scale-up
- Contract manufacturing
By staying up to date on current pharma market insights, Oakwood Labs can help deliver the pharmaceutical solutions you’re looking for.
Contact Oakwood Labs for More Information
Oakwood Labs is a global provider of sustained-release pharmaceuticals and other medical services. Please contact our team of experts today for more information about all we can provide, as we look forward to answering any inquiries you have.
At Oakwood Labs, we’re dedicated to providing alternative solutions to drug delivery and development. This includes our ongoing work creating long-acting injectables for treating pulmonary arterial hypertension.
For those interested in learning more about the specific strides we’ve made within this sector, as well as the opportunity to partner with us, read on or contact our team today.
Then and Now: A Brief History of Pulmonary Arterial Hypertension Drug Development
The introduction of Epoprostenol in 1995 marked the first true breakthrough in pulmonary arterial hypertension (PAH) treatment, as this medication was able to show the potential to target the prostacyclin pathway. Following this development, individuals began further research into other potential treatment options to help patients suffering from PAH.
It was not until 2001 that the first oral therapy, Bosentan, was approved and released to the public. Since then, 12 additional medications have been approved by the FDA to treat PAH, such as soluble guanylate cyclase (sGC) stimulators, endothelin receptor blockers (ERBs), and phosphodiesterase-5 (PDE-5) inhibitors, to name a few.
Additionally, there are a few current trends in the advancement of pulmonary arterial hypertension pharmaceutical development, including those focused on:
- Combination therapies
- Targeted therapies
- Delivery methods
About Our Work Creating Long-Acting Injectables for Treating Pulmonary Arterial Hypertension
The team at Oakwood Labs has used its advanced technology to create injectables for treating pulmonary arterial hypertension. Though most of the formulations that are currently on the market for PAH treatment are mainly oral medications, the use of LAIs can come with several advantages, such as a decrease in the amount of drug administered to the patient, less frequent doses, and more.
Partner with Oakwood Labs
In order to further develop our cardiology program, Oakwood Labs is looking for an external partner to fulfill the responsibilities of the role. This includes managing phases 1–3 of clinical trials, funding development activities, and helping with ongoing commercialization and registration efforts.
For more information on the details of the position, please reach out to our team directly, as we would be happy to supply you with additional information about the development work to date, market opportunity, and estimated financial projections.
FAQs About Pulmonary Arterial Hypertension LAI Development
What are the major benefits of an LAI in cardiovascular treatments?
Pulmonary arterial hypertension (PAH) is a rare, progressive disease that causes high blood pressure in the arteries of the lungs. Symptoms include shortness of breath, chest pain, and increased heartbeat.
LAI treatments in this area focus on vasodilators and platelet aggregation inhibitors. They work by relaxing blood vessels, including those in the lungs, and improving blood flow.
What are the current barriers to an LAI entering this particular space?
The barriers to entry for the LAI space are very high. You need to have a proven technology capable of delivering the right amount of the drug within a given therapeutic window. Plus, you need an FDA-approved GMP facility to manufacture the product, as well as a high level of expertise to understand, develop, and validate the process.
Oakwood Labs has all of these capabilities and over 25 years of experience within this field.
What sets Oakwood Labs apart from others in the development of LAIs to treat PAH and other cardiovascular issues?
Our team of experts has used its technology to develop formulations focused on treating pulmonary arterial hypertension with a release duration of one month. Current treatments, which mostly focus on oral medications, work in different ways but ultimately attempt to decrease symptom severity and increase exercise capacity.
The use of an LAI product would offer benefits similar to other therapeutic areas including reduction in the total amount of drug administered to the patient, as well as less frequent doses.
Reach Out to Us
If you have any additional questions about our continued work in pulmonary arterial hypertension drug development, or if you’re looking to partner with us, please contact us today.
The team at Oakwood Labs has made it our mission to develop long-acting injectables to treat various diseases and disorders. This includes ongoing work with drugs to treat acromegaly and carcinoid tumors, both rare diseases that affect millions of people globally. Read on to learn more about the strides we’ve taken within endocrinology, and the broader healthcare sector.
The History of Acromegaly and Carcinoid Tumor Drug Development
Though carcinoid syndrome was first described by Thorson and colleagues in 1954, Pierre Marie discovered acromegaly years prior in 1886. At these times, there were no acromegaly and carcinoid tumor pharmaceuticals to reduce the size of malignant or benign growths, so surgical removal of a tumor was incredibly common.
Then, in the 1970s, dopamine agonists, such as bromocriptine and cabergoline, were introduced as treatment options to control tumor growth for acromegaly and carcinoid syndrome. However, the treatment came with a range of side effects, such as nausea, dizziness, and constipation, to name a few, so they are not used as standalone options for treatment today.
The Current State of These Pharmaceuticals
Numerous strides have been made within the healthcare sector since the early stages of acromegaly and carcinoid tumor drug development. For example, as of June 2020, the FDA has approved oral octreotide capsules as one of the first long-term maintenance treatments for acromegaly. This alternative is a viable solution for individuals who have responded to and tolerated treatment with injectable SRLs.
Along with more recent trials and discoveries, several targeted drugs are used to treat these diseases and manage their symptoms, with Sandostatin being one of the most common. These synthetic acromegaly and carcinoid pharmaceuticals are designed to mimic the body’s natural hormone, somatostatin, which, in turn, prevents the body from producing too many growth hormones and serotonin.
What Oakwood Labs Is Developing Internally for Acromegaly and Carcinoid Tumor Treatment
Oakwood Labs has successfully manufactured and scaled up formulations focused on treating acromegaly and carcinoid tumors. The daily injections initially used for these conditions have been largely replaced by Sandostatin LAR, a one-month LAI product. Plus, our two-month formulations further reduce the number of injections and office visits patients experience by 50%, which can also help with enhancing patient compliance.
Additionally, Oakwood Labs currently has two endocrinology programs that are focused on creating pharmaceuticals to treat acromegaly and carcinoid tumors. Project Treestar is designed to specifically treat acromegaly and cancer-related nausea, while Project Lunar is looking to help those with type 2 diabetes.
Partnership Opportunities
Oakwood Labs is seeking an external partner to help further develop our endocrinology program. Just some of the key responsibilities include:
- Funding the ongoing development activities
- Overseeing phase 1-3 of clinical trials
- Contributing to registration and commercialization efforts
If you’re interested in pursuing this opportunity, please reach out to our team directly for more information. We would be happy to supply the partner with additional information about the market opportunity, estimated financial projections, and development work to date.
FAQs About LAIs for Acromegaly and Carcinoid Tumor Treatment
What are the major benefits of an LAI in treatments for acromegaly, carcinoid tumors, and more?
When developing drugs for treating acromegaly and carcinoid tumors, know that long-acting injectables are effective for blocking the production of excess blood levels of growth hormone (GF) and reducing the insulin growth factor-1 (IGF-1) levels in acromegaly patients. This is helpful for individuals who cannot be treated with other methods, such as surgical intervention.
Sandostatin acts as a somatostatin analogue, mimicking a naturally occurring hormone that helps regulate hormone release from the tumor cells. This aids in the treatment of carcinoid tumors.
What are the current barriers to an LAI entering this particular space?
The barriers to entry for the LAI space are very high. You need to have a proven technology capable of delivering the right amount of the drug within a given therapeutic window. You also need an FDA-approved GMP facility to manufacture the product. Finally, you need a high level of expertise to understand, develop, and validate the process.
Oakwood has all these capabilities, along with over 25 years of expertise within the field.
Contact Our Team of Experts Today
If you have any questions regarding the process of developing pharmaceuticals for treating acromegaly and carcinoid tumors, or our work in the endocrinology space, please reach out to our team of experts today. And if you’re looking for a position within our partnership program, contact us directly, as we look forward to hearing from you.
Opioid abuse disorder is very common, affecting over 20 million people worldwide and over 3 million people in the United States. People who misuse opioids may also advance to even more harmful drugs such as heroin, making this a critical issue that needs to be addressed. With the help of long-acting injectables for opioid use disorder pharmaceutical development, new treatment options are now available to patients that are more sustainable.
The History of Opioid Use Pharmaceuticals
The first modern opioid crisis began in the 19th century. During and after the Civil War, this opioid crisis emerged as soldiers were given substances to treat their wounds, pain, PTSD, and depression. As a result, many soldiers developed an opioid addiction. Doctors at this time would give a patient morphine because it was a general cure for all chronic pain problems, but it obviously had negative effects as well.
The opioid crisis dwindled by 1900, and for roughly 90 years opioids were only abused by smaller groups of people. It wasn’t until the early 2000s that the use of opioids once again began affecting communities all over the country. While doctors started to notice the spread of opioids and took steps to curtail it, people were finding other ways to illegally acquire the drugs.
While there are still issues today, we have grown more aware of the risks that are associated with opioid use. There are many efforts being made to hopefully reduce instances of abuse, such as educating those on alternate pain management strategies, developing abuse-deterrent formulations, having stricter prescription guidelines in place, and offering opioid use disorder pharmaceutical development.
Benefits of Long-Acting Injectables for Treating Opioid Use Disorder
Long-acting injectable, or LAI, formulations ensure that patients receive their medications on a regimented schedule. Drugs such as naltrexone and buprenorphine are formulated as monthly injections in order to block the effects of opioids. Initially, these drugs were formulated in daily oral dosages, but LAI products are more effective, as they result in greater patient compliance.
In addition to improved compliance, injectables to treat opioid abuse disorder provide benefits such as:
- Ability to target specific anatomical areas – LAI buprenorphine targets the receptors in the brain, providing effects that help control withdrawal symptoms, reduce cravings, block the euphoric effects of opioids, and maintain stable blood concentrations without peaks.
- Helping to prevent drug abuse – By receiving long-acting injections, patients eliminate the need for daily dosing, reducing the risk of missed doses and relapses.
- Potential for improved outcomes – Injectables help reduce the opportunities for misuse and ensure consistent medication levels are maintained, possibly leading to better outcomes for the patient.
How Oakwood Labs Stands Out
Oakwood Labs has developed 2-, 3-, and 4-month duration prototype formulations of naltrexone, using a different polymer than is used in the 1-month duration naltrexone. We are currently working on scaling up these formulations prior to clinical trials.
We also have a track record of success in bringing other projects from proof of concept to clinical trials, such as proving the duration of release of naltrexone formulations in animal PK models. We are currently seeking partners for clinical development.
By choosing us as a partner in developing injectables to treat opioid use disorder, you’ll benefit from:
- Strong communication and project management that achieves milestones
- Patented microsphere technology that allows tailored release profiles from weeks to one year
- Over 20 years of experience encapsulating sustained-release injectables
- A full-service operation, from R&D formulation development through GMP commercial manufacturing
- An FDA-approved aseptic GMP facility manufacturing clinical and commercial sterile injectables
FAQs on Injectables to Treat Opioid Use Disorder
How do these medications work?
Naltrexone helps block the sedative and euphoric effects of drugs such as codeine, morphine, and heroin. This medication is reported to reduce opioid cravings. Buprenorphine, on the other hand, helps avoid withdrawal symptoms and manage cravings.
What are the current barriers to an LAI entering this particular space?
It is difficult to develop LAI formulations of these drugs, especially for formulations in excess of one month in duration of release. Currently, 1-month duration products have been approved, but no longer than 1-month duration products have been approved yet. Some people are working to develop longer duration products, such as a 2-month duration naltrexone and a 3-month duration buprenorphine. It is generally accepted that longer duration products would be beneficial for patient compliance.
Who are good candidates for injectables?
People who may benefit from injectables for treating opioid use disorder and other conditions include:
- Those who are high-risk, meaning they experience frequent hospitalizations or multiple relapses
- Those who prefer less frequent dosing
- Those who are nonadherent to oral antipsychotics
- Those experiencing dose-dependent adverse effects
- Those who have poor oral absorption
Besides opioid use disorder, what else can LAIs help treat?
Long-acting injectables have been used to treat a variety of conditions such as schizophrenia, bipolar disorder, depression, and more. LAIs have also been used as pharmaceuticals which offer numerous benefits for oncology treatment.
Choose Oakwood Labs for Opioid Abuse Disorder Pharmaceutical Development
If you have an interest in long-acting injectables for treating opioid use disorder, please reach out to us today. We look forward to providing you with more information on how to tackle this ongoing issue in today’s world.
Oakwood Labs will be exhibiting at Booth #31 and speaking at the upcoming 2024 PODD Conference taking place from October 28-29 in Boston. If you would like to learn more about the event and register to attend, please visit the following link: https://poddconference.com/
Company Overview
Oakwood Labs is a global leader in sustained release drug delivery. We support all phases of long acting injectable development from initial feasibility studies through FDA-approved clinical and commercial supply. Oakwood has 27 years of drug encapsulation experience using Chroniject™, our patented microsphere-based technology. Chroniject™ provides the ability to control particle size, customize release durations from weeks to years, and minimize residual solvents to achieve critical quality attributes.
Listen to Oakwood’s presentation during Day 1 on our Chroniject Technology: A Solution to Long Acting Injectable Formulation and Scale-Up Challenges
Colin Spencer, a project manager working within our technology transfer team will be presenting during Day 1 (Monday, October 28th) of the conference within the Track 1A: Injectable Formulations & Technologies at 2:30pm.
The presentation will include the following key points:
- Oakwood’s Chroniject technology provides a tunable long-acting injectable platform for a wide array of molecules and applications. Efficacious release profiles have been generated from as fast as two days to as long as one year.
- Oakwood’s Chroniject technology provides the platform for scale-up of the formulation process, allowing for the critical quality attributes of the long-acting injectable formulations to be maintained from initial feasibility batch sizes in the gram-scale to clinical and commercial batch sizes in the kilogram-scale.
Stop by Oakwood Lab’s Booth #31 to meet our team and learn more about how we can assist in the following areas:
- Long Acting Injectable Patented Technology (CDMO Services)
- Feasibility assessments
- Scale-up and optimization of lead formulation
- Manufacturing, characterization, and stability of R&D toxicology batches
- GMP Clinical trial manufacturing (Phase I, II, III)
- GMP Commercial manufacturing
- Contract Manufacturing (CMO Services)
- Technology Transfer
- GMP Registration and Validation batches
- Aseptic GMP commercial batch manufacturing
- ICH compliant stability testing
Contact Us for More Information
PODD 2024 conference covers a wide range of topics, and we are happy to contribute to the event! If you aren’t able to attend, but still want to learn more about Oakwood Labs or what you missed at the conference, contact us today!
We look forward to discussing our technology and more.
Oakwood Labs is happy to announce that we will be exhibiting at Booth #2610 at the upcoming 2024 AAPS PharmSci 360 on October 20-23 in Salt Lake City, Utah. If you would like to learn more about the event and register to attend, please visit the following link: https://www.aaps.org/pharmsci/annual-meeting
Company Overview
Oakwood Labs is a global leader in sustained release drug delivery. We support all phases of long acting injectable development from initial feasibility studies through FDA-approved clinical and commercial supply. Oakwood has 27 years of drug encapsulation experience using Chroniject™, our patented microsphere-based technology. Chroniject™ provides the ability to control particle size, customize release durations from weeks to years, and minimize residual solvents to achieve critical quality attributes.
Stop by Oakwood Lab’s Booth #2610 to meet our team and learn more about how we can assist in the following areas:
- Long Acting Injectable Technology (CDMO)
- Feasibility studies
- Scale-up of formulation
- Manufacturing toxicology batches
- Clinical trial manufacturing (Phase I, II, III)
- Contract Manufacturing (CMO)
- Technology Transfer
- GMP Registration and Validation batches
- Aseptic GMP commercial batch manufacturing
- ICH compliant stability testing
Contact Us for More Information
The AAPS 2024 conference covers a wide range of topics, and we are happy to contribute to the event! If you aren’t able to attend, but still want to learn more about Oakwood Labs or what you missed at the conference, contact us today!
We look forward to discussing our technology and more.
Joint pain affects many people around the world, creating problems with everyday tasks, causing discomfort, and lessening their quality of life. Fortunately, advances in medicine have led to relief for those who suffer from a variety of conditions that result in joint pain, with long-acting injectables being an efficient method of delivery.
At Oakwood Labs, we’re a leader long-acting injectable development, putting our proven methodologies to work in drugs to treat joint pain. Read on to learn more about joint pain drug development and how the Oakwood Labs team can supply exactly what your operations need.
The History and Use of Long-Acting Injectables for Joint Pain Pharmaceuticals
Long-acting injectables were created in the 1950s to aid patients suffering from mental health conditions such as schizophrenia. As procedures evolved and new developments arose in the ensuing decades, the treatment of other conditions, including those centered more on the total body rather than just the mind, began to emerge. This includes using long-acting injectables to administer drugs for treating joint pain in knees, elbows, shoulders, and other problem areas.
Some of the common conditions that are suited for long-acting injectable medication distribution include:
- Osteoarthritis
- Rheumatoid arthritis
- Bursitis
- Tendonitis
- Psoriatic arthritis
Meanwhile, there are a range of medication types that may be distributed. These can include osteoarthritis pharmaceuticals, rheumatoid arthritis pharmaceuticals, and other forms, with specific injections containing:
- Corticosteroids
- Hyaluronic acid
- Platelet-rich plasma
- Additional formulations
Key Benefits of Long-Acting Pharmaceutical Drugs to Treat Joint Pain
Long-acting injectables, sometimes referred to as extended-release drugs or “ER drugs,” help to provide ongoing pain relief to patients who are suffering from an array of conditions. The result is a better quality of life, better pain management, increased mobility, and fewer dosages. Other benefits of these pharmaceuticals for treating joint pain include:
- Fewer side effects – Using long-acting injectable pharmaceuticals to treat joint pain can result in fewer side effects for patients because they will receive less frequent dosages than with immediate-release approaches. The reduced side effects are also facilitated by patients receiving lower peak concentrations of the given drug.
- Improved patient compliance – Since long-acting joint pain pharmaceuticals necessitate fewer doses, patients who take them are more likely to follow the plan put in place by their healthcare professionals. This results in improved pain management and happier patients.
- Reduced pain level fluctuations – Patients who take immediate-release drugs may notice a fluctuation in pain levels for their joint issues, but long-acting injectables lessen this experience, offering a more stable and controlled release that manages pain.
Our Abilities in Joint Pain Drug Development
The Oakwood Labs team has been proud to tackle projects for osteoarthritis drug development and rheumatoid arthritis drug development, providing long-acting injectables with a release duration of three months.
Our team specializes in developing pharmaceuticals that treat joint pain and can assist with developing formulations, scaling up the manufacturing process, and manufacturing clinical and commercial quantities under GMPs.
We find that long-acting injectables are ideal for use with pharmaceuticals for treating joint pain because joint pain often emanates from a specific bodily area and high concentrations of a drug can be administered without resulting in systemic exposure. This, and the potential for disease-modifying results, are yet more benefits to the LAI approach.
Our Work with LAI Formulations
In terms of our work, Oakwood has developed a 3-month LAI formulation of meloxicam. Meloxicam is one of the more potent NSAIDs, which enables targeted release in the intra-articular space, and thus avoids the systemic side effects of NSAIDs. Due to the high potency of meloxicam, a smaller injection volume is possible.
Challenges We Have Faced
One of the current barriers to entering this particular space is the difficulty of developing the proper formulation. Microspheres are preferable to gels that solidify after injection due to the mechanics of the joint and intra-articular space. Microspheres should be greater than 20 microns to avoid macrophages attacking them. Work with our team of LAI experts to develop the right formulation.
Partner with Us on Drugs to Treat Joint Pain
Oakwood Labs is actively looking to partner with interested organizations for co-development of programs such as those focused on treating joint pain. Be sure to visit our partnership page for more information on our approach and all areas we focus on. We would love to work with you to bring new drugs to market.
Have Questions About Pharmaceuticals to Treat Joint Pain? Contact Us
Reach out to the team at Oakwood Labs today and we can discuss our methodologies, facilities, previous projects, and more. We look forward to hearing from you.
At Oakwood Labs, we’re proud to contribute to the development of cancer pharmaceuticals through our continuous work manufacturing long-acting injectables (LAIs). That’s why we’ve compiled an informational guide showcasing our ongoing work in the healthcare field, as well as the numerous benefits of LAIs for oncology treatment.
Advantages of Long-Acting Injectables to Treat Cancer
There are numerous advantages to the use of LAIs as pharmaceuticals to treat cancer. To start, Bruton tyrosine kinase (BTK) inhibitors are established standards of care in multiple B-cell malignancies including chronic lymphocytic leukemia, mantle cell lymphoma, and Waldenstrom macroglobulinemia. LAI formulations of BTK inhibitors offer certain advantages in terms of pharmacokinetics (PK) and patient adherence. For example, ibrutinib (Imbruvica) has a very short half-life of 4-6 hours. Hence, relatively large doses of the oral form are required to target plasma levels within the therapeutic range.
The PK profile is marked by large peaks and valleys, sometimes exceeding the therapeutic level, and sometimes falling below. The PK profile of the LAI formulation is much “smoother,” having no significant peaks and valleys. Also, the oral bioavailability of ibrutinib is only 3% and varies among patients. The LAI formulation, meanwhile, is 100% bioavailable and therefore can be administered at much lower per-day doses.
These factors above could reduce side effects caused by off-target receptor interactions, while maintaining efficacy, and result in fewer cases in which the medication needs to be discontinued. The LAI formulations of two weeks and one month ensure patient adherence for these periods, possibly enhancing efficacy in clinical practice.
Similar benefits may be possible with other immunomodulatory cancer pharmaceuticals, such as the thalidomide analog pomalidomide (Pomalyst), indicated for multiple myeloma. The recommended dose for multiple myeloma is 4 mg per day taken orally on days 1 through 21 of repeated 28-day cycles. The half-life is approximately 7.5 hours and oral bioavailability is estimated to be approximately 75%. The LAI formulation reduces the peaks and valleys of drug exposure, enables a reduction in the total amount of drug administered, reduces the frequency of doses, possibly reduces side effects, and ensures patient adherence.
Additional Benefits to Highlight
Along with administration approaches and the long-term effects on the body, LAIs as oncology pharmaceuticals possess several key advantages for the patient, including:
- Reduced treatment burden
- Increased patient compliance
- Sustained stable hormone suppression
How Oakwood Labs Is Contributing to Cancer Drug Development
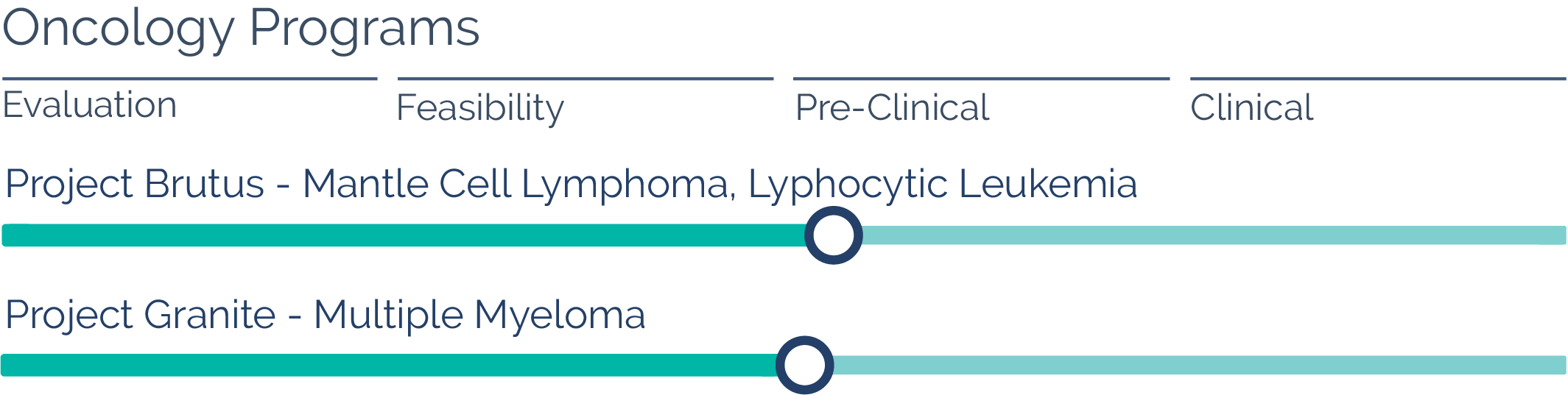
Alongside working with external partners who have been seeking out LAIs for their own initiatives, our team is also currently in the process of creating internal programs that utilize our very own microparticle technology. The goal of these internal initiatives is to convert an existing product into an LAI formulation to extend the duration of drug release to what is currently on the market, achieving patient compliance and ease of use.
More specifically, Oakwood Labs has used its internal technology to progress its formulations that are focused on treating mantle cell lymphoma, small lymphocytic lymphoma, chronic lymphocytic leukemia, and multiple myeloma with release durations ranging anywhere between two and four weeks. Our LAI oncology drug development has led to significant benefits for patients, such as:
- Reducing the amount of drug administered to the patient
- Decreasing the number of doses needing to be injected
- Diminishing more adverse reactions and side effects from dosages
Partnership Opportunities
At this point in the cancer drug development process, our team is actively seeking an external partner to help further develop our internal program. Key responsibilities in this area include funding ongoing development activities as well as phases one through three of clinical trials and registration/commercialization efforts.
If you’re interested in learning more about this opportunity, please contact our team directly, as we would be happy to provide additional details or answer any questions you may have.
FAQs About Oncology Pharmaceuticals, Development, and More
Can you provide me a brief history of oncology pharmaceutical development and its breakthroughs?
Though it is estimated that the preliminary study and treatment of cancer was initially recorded as early as 520 BCE when Persian queen Atossa was treated for a breast tumor, modern-day pharmaceuticals for treating cancer did not surface until relatively recently. Just some of the pivotal findings in this scientific journey include:
- The 1840s – Physician Rudolf Virchow is well-known for his observation of cancer cells during this time, in which he defined their key characteristics. This led to the future of cancer treatment protocols by the start of the 20th
- 1895 – Once German physicist Wilhelm Conrad Röntgen first correctly identified the waves of radiation that we all now know as X-rays, this equipment was then used in radiotherapy cancer treatment shortly thereafter.
- The 1940s – Based on the discovery that nitrogen mustard contains anticancer properties during World War II, researchers were able to develop various cytotoxic drugs to directly target dividing cancer cells, which later led to today’s chemotherapy practices.
Can you tell me more about the work Oakwood Labs does to develop LAIs?
Oakwood Labs performs LAI development through our technology platform Chroniject™, and some characteristics of products we have made with this system including the following:
- The duration of release is one week to one year
- LAIs are easily syringable with 18- to 23-gauge needles
- Products are reconstituted immediately with sterile water
- LAIs are filled aseptically and terminally sterilized if feasible
- Products have proven content uniformity and good stability characteristics
- LAIs are free of foreign particulate matter
Additionally, Chroniject™ is microsphere-based and has biodegradable polymers such as PLA, PLGA, and other polymers with demonstrated low toxicity and sourced from multiple suppliers. Plus, the finished dosage form typically consists of a lyophilized vial containing microspheres, a suspending agent, and other excipients.
What are the current barriers to an LAI entering this particular space?
The barrier to entry is that LAI formulations are extremely difficult to develop and require a high degree of technical expertise. Once developed, you then need to scale up the process to be able to manufacture in an aseptic GMP facility. The Oakwood Labs team can work with you to overcome key challenges.
What are some common trends in the development of drugs to treat cancer?
As healthcare professionals and pharmaceutical developers continue to produce different types of drugs for treating cancer, numerous trends have emerged from their discoveries, such as:
- Targeted drugs for treatment
- Immunotherapy
- Monoclonal antibodies
- Small molecule-targeted agents
- CRISPR
- Biomaterials, such as chitosan oligosaccharide (COS)
These recent practices have significantly advanced the oncology field, leading to longer, happier, and healthier lives for patients undergoing treatment.
Contact Oakwood Labs for More Information
If you have any additional questions about the oncology drug development process, or if you’re looking to get in touch with us regarding a potential partnership opportunity, please contact our team today. We look forward to assisting you.